
3 Blood Tests Can Warn Women of Risk 30 Years before Heart Attack and Stroke

Posted on September 10, 2024
Ronald Grisanti D.C., D.A.B.C.O., DACBN, MS, CFMP
New paper published in the New England Journal of Medicine has found that three important cardiovascular lab tests have the potential to warn women of potential future heart attacks and strokes 30 years early.
Unfortunately the standard of medical care almost always includes checking total cholesterol and LDL but does not commonly include two additional critical cardiovascular lab tests.
These two additional labs are high sensitivity C-Reactive Protein (CRP) and Lipoprotein (a) -Lp(a)
C-reactive protein (CRP)
C-reactive protein (CRP) is a substance found in the blood that increases when there is inflammation within your body. The high-sensitivity C-reactive protein (hs-CRP) test is more sensitive than the standard CRP test measuring slight increases in CRP levels even when within the normal range. Because of this greater sensitivity, the hsCRP test can help determine your risk of cardiovascular disease (CVD).
Lipoprotein (a)
Lp(a) is a large lipoprotein made by the liver. Lipoproteins are parcels made of fat and protein. Their job is to carry fats (also called lipids) around the body in the blood. LDL cholesterol (or ‘bad cholesterol') is also a lipoprotein.
Lp(a) is made of:
- a lipoprotein similar to LDL (low density lipoprotein or "bad" cholesterol)
- plus two proteins known as ApoB and Apo(a).
A high level of Lp(a) in the blood has now been identified as a risk factor for cardiovascular disease or CVD. It can cause atherosclerosis (furring up of arteries), heart attacks, strokes, peripheral arterial disease, aortic valve disease and heart failure.
Genetic factors play a major role in Lp(a) concentrations. In fact, Lp(a) levels are 70% to 90% genetically determined.
There are also ‘secondary causes' that can affect your Lp(a) levels. These include conditions such as chronic kidney disease (CKD), nephrotic kidney disease and hypothyroidism.
Statins do not lower the amount of Lp(a) but they will shrink the size of the Lp (a) lipoproteins.
Ordering CRP and Lipoprotein (a)
C-Reactive Protein (CRP) High Sensitivity (Cardiac)
- LabCorp code: 120766
- Quest code: 10124
Lipoprotein (a)
- LabCorp code: 120188
- Quest code: 34604
The study found that a blood test that evaluates levels of three compounds — Lipoprotein (a), high sensitivity C-Reactive Protein, and LDL cholesterol — can accurately reveal heart disease in the making.
Women in their fifties with the highest levels of these three substances were 3 times more likely to develop heart disease over the next 30 years than women with the lowest levels.
The New England Journal of Medicine Study
The study consisted of collecting blood samples and detailed medical information from about 28,000 women when they were in their mid-fifties, then followed them for 30 years. During the study period, over 3,500 participants had a heart attack, stroke, surgery to restore circulation, or died of cardiovascular-related causes.
Women with the highest levels of LDL cholesterol were 36 percent more likely to experience these cardiovascular events than participants with the lowest LDL levels.
Similarly, the risk of these events was increased by 33 percent for women with the highest lipoprotein(a) levels.
More worrisome was the fact that women with the highest C-reactive protein levels saw their risk of heart disease increase by 70 percent compared with women with the lowest levels.
In addition, women with the highest levels on all three lab tests were almost 3 times more likely to develop heart disease and about 1.5 times more likely to experience a stroke than participants with the lowest results on these three tests.
Optimal Healthy Levels of Lipoprotein (a)
A normal lipoprotein (a) level for adults is less than 30 milligrams per deciliter (mg/dL) of blood. Levels above this are considered abnormal and are categorized as follows:
- Borderline risk: 14 to 30 mg/dL
- High risk: 31 to less than 50 mg/dL
- Highest risk: Greater than 50 mg/dL
Optimal Healthy Levels of High Sensitivity C-Reactive Protein
The optimal level of high sensitivity C-reactive protein (hs-CRP) is less than 1.0 mg/dL, which is considered low risk for cardiovascular disease. Levels between 1.0 mg/dL and 3.0 mg/dL are considered average risk, and levels higher than 3.0 mg/dL are considered high risk.
How to Lower High Sensitivity C-Reactive Protein
1: Rule Out the Below Underlying Health Conditions
- Infection: Bacterial, fungal, and bone infections, such as sepsis and osteomyelitis, can cause high CRP levels.
- Autoimmune disorders: Rheumatoid arthritis, lupus, and certain types of inflammatory bowel disease (IBD), such as Crohn's disease and ulcerative colitis, can cause high CRP levels.
- Cancer: Cancer can cause high CRP levels.
2: Exercise
Exercise reduces CRP both directly by reducing cytokine production in fat, muscle, and mononuclear cells, and indirectly by increasing insulin sensitivity, improving endothelial function, and reducing body weight.
3: Weight Loss
In those who are overweight and obese, weight loss and fat reduction have reduced CRP levels.
- A study found that for each kilogram of weight lost, CRP levels decreased by an average of 0.13 mg/L.
- One study found that the odds of achieving desirable CRP levels more than doubled with 5% loss of total body weight and fat mass.
- Other studies indicate that fat stored in the abdomen and thigh muscles is associated with higher levels of CRP independent of total fat mass, suggesting that greater reduction of fat in these regions may be associated with greater improvement in CRP levels.
4: Mediterranean/Plant-Based Diet
Diets high in fiber and rich in fruits and vegetables are associated with lower CRP levels, while a Western diet and diets high in fat, sugar, and refined grains can increase CRP.
- High dietary fiber intake, in particular, has been associated with lower CRP levels.
- In one study, participants received a 45% fat 1,000 Kcal Mediterranean-like meal (monounsaturated 61% of fat) or a Western-like meal (saturated 57% of fat). The Mediterranean-like meal resulted in a decrease in CRP 2 hours after eating.
5: Yoga, Tai Chi, Qigong, and Meditation
Studies suggest that 7 to 16 weeks (1–3 hrs weekly) of these “mind-body therapies” can cause significant improvements in CRP levels.
6: Optimism
In a study with over 6,800 people, inflammatory markers including CRP were increased in those prone to pessimism.
7: Green Tea
Green tea may lower CRP levels by inhibiting the nuclear factor kappa-light-chain-enhancer of activated B cells (NF-kB). Studies have found that green tea extract reduces inflammatory biomarkers including CRP.
8: Supplements
Note: Always discuss the following supplement recommendations with the physician and/or functional medicine healthcare provider.
Research has shown the following may help decrease CRP levels:
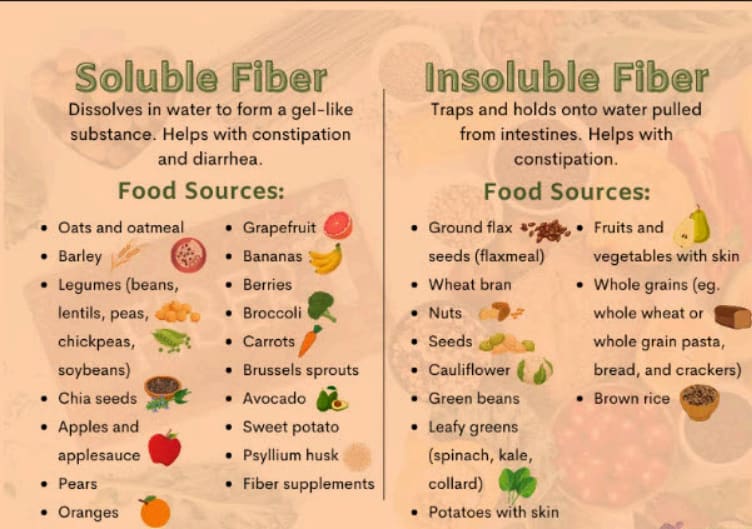
Fiber: A combination of both soluble and insoluble fiber should be consumed per day to effectively lower CRP. Total dietary fiber intake should be 25 to 30 grams a day from food.
Cocoa and dark chocolate
A study found that subjects who consumed up to 20 grams of dark chocolate every three days had lower serum hs-CRP concentrations than non-consumers.
Folate
Folic acid supplementation reduced serum levels of CRP in adults, particularly in trials that prescribed folic acid at doses less than 5mg/d for more than 12 weeks.
I suggest taking a methylated folic acid if you have the MTHFR gene.
Labcorp offers a Methylenetetrahydrofolate Reductase (MTHFR) C677T and A1298C paired test. The Labcorp code: 511238.
Magnesium
Studies have shown that higher magnesium intake is associated with lower CRP levels. For example, one study found that CRP concentrations were 12% lower in the highest magnesium intake quintile than in the lowest.
Omega-3
Omega-3 fatty acids (omega-3 PUFAs) can lower C-reactive protein (CRP) by reducing the production of eicosanoid mediators that cause inflammation. Omega-3 PUFAs also decrease the levels of other pro-inflammatory markers, such as tumor necrosis factor (TNF)-α and interleukin (IL)-6.
Vitamin C
In this University of California at Berkeley study, participants who received vitamin C and started out with C-reactive protein levels greater than 2.00 mg/L had 34% lower levels compared with the placebo group after only two months.
Lp(a) and Genetics
Having an elevated Lp(a) is almost entirely determined by the genes you inherit. Lp(a) levels are 70% to 90% genetically determined. Unfortunately, lifestyle changes such as diet and exercise do not reduce Lp(a), and most of the commonly used preventive strategies for those with risk factors for CVD are ineffective.
** NOTE: Although lowering Lp(a) may in fact be challenging, to say the least, there are things you can to do to possibly nudge the Lp(a) down. It is highly unlikely that one with an elevated Lp(a) will ever get it to a normal range. However the vast majority of respected cardiologists encourage those with elevated Lp(a) to do everything they can to optimize ALL of the other cardiovascular markers. These would include: Total cholesterol, LDL cholesterol, LDL-C, LDL-P, LDL Small particle size, Triglycerides, ApoB, Homocysteine,(Lp-PLA2) Activity, etc.
Also be certain you maintain a normal and optimal blood pressure and stay lean.
Potential Strategies to Lower Lp(a) and LDL Cholesterol
- Mediterranean diet may help mediate the association between lipoprotein-alpha (Lp(a)) and cardiovascular disease (CVD) risk. However, Lp(a) levels are primarily determined by genetics and are usually unaffected by diet, lifestyle, or environment, however as mentioned above this recommendation and the ones below will indeed go a long way to improve other cardiovascular risk markers.
- Avoiding sugary foods and sweetened drinks
- Drinking alcohol in moderation
- Eating foods that lower cholesterol, such as oats and foods fortified with plant stanols and sterols
- Maintaining a healthy weight
- Keeping blood pressure under control
- Getting regular exercise
- Refraining from smoking or vaping
Some medications that can help lower lipoprotein (a) include:
PCSK9 inhibitors: Found to reduce lipoprotein(a) concentration by 20% to 25%
Women Hormone Replacement Therapy (HRT)
Postmenopausal hormone replacement therapy can lower Lp(a) levels by approximately 20–25%. A systematic review and meta-analysis of 10 clinical trials, which included 2049 postmenopausal women, suggested that anti-estrogen therapy significantly reduced Lp(a) levels by approximately 5.92%.
NOTE: If you decide to consider HRT I first and foremost recommend consulting with a healthcare provider knowledgeable in HRT and will check your hormones with one of the following two hormone tests
https://rheinlabs.com/
https://dutchtest.com/
Aspirin: Low-dose aspirin can help reduce lipoprotein (a)
Statins: While statins don't lower lipoprotein (a) levels, they can shrink the size of the lipoprotein and lower non-HDL cholesterol levels.
NOTE: If one has applied the information in this article and still has elevated LDL Cholesterol and other elevated lipid markers a statin may be necessary. Unfortunately there are those that discount the significance of lowering LDL cholesterol and claim that high levels are fine. I adamantly disagree and will say with much boldness that you are putting yourself at a high and dangerous risk if you do not do everything you can to lower your LDL cholesterol to optimal levels.
Here are the other LDL cholesterol ranges:
- Optimal: less than 100 mg/dL
- Borderline high: 130 to 159 mg/dL
- High: 160 to 189 mg/dL
- Very high: 190 mg/dL and higher
**If you have a history of heart attack or stroke, or are on cholesterol-lowering medication, your doctor may aim for an LDL level of 70 mg/dL or lower. People with a history of atherosclerosis may also want to aim for an LDL level below 70 mg/dL.
Some studies suggest that lowering LDL cholesterol levels can help reverse atherosclerosis, and that a level of less than 70 mg/dL can reduce plaque progression by up to 24%
Lipoprotein apheresis
Lipoprotein apheresis is a procedure that removes lipoproteins from the blood to treat high cholesterol and other conditions. Lipoprotein apheresis can lower LDL and Lp(a) by 70 percent. It can also decrease inflammatory markers, coagulation factors, and fibrinolytic proteins This is the only FDA-approved therapy for lowering lipoprotein (a) in the United States
How it works: A patient is connected to a machine that separates the plasma from the blood and removes LDL and Lp(a). The blood is then returned to the patient.
When it's used: Lipoprotein apheresis is used when lifestyle and drug treatments aren't effective. It's often used as a "last resort" therapy for dyslipidemias.
How often it's used: Treatments are usually once every two weeks and last 2-3 hours
Supplements and Nutraceuticals That MAY Help Lower Lp (a)
Niacin (Must be Nicotinic acid): Can lower lipoprotein (a) levels by 25-40%
Nicotinic acid, also known as niacin, is the form of niacin that lowers cholesterol. Other forms of niacin, such as nicotinamide and inositol nicotinate, do not lower cholesterol
The following is one of my patients who was prescribed 1000 mgs of Niacin CRT (Nicotinic acid) from Designs for Health before bed.
It is important to take before bed. As you can see the patient's Lipoprotein (a) improved 94 points from 222 to 132 in six months.
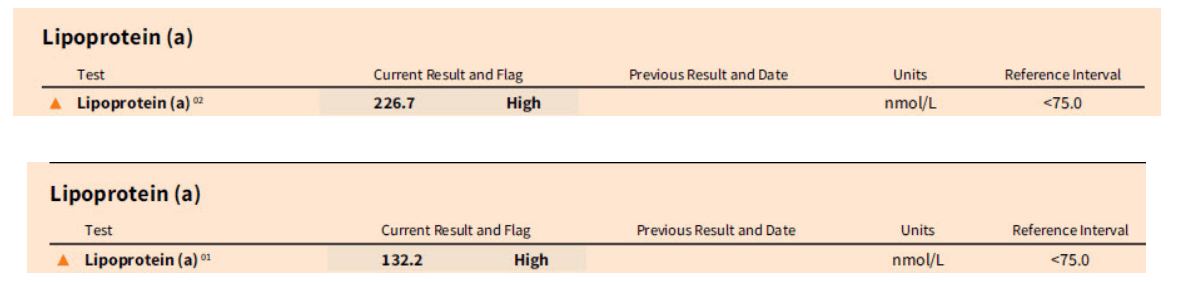
** Some patients are unable to handle the flushing commonly associated with taking Nicotinic acid. It is also important to have your liver enzymes checked every three months because niacin may cause an increase.
Supplements like L-carnitine and ascorbic acid combined with L-lysine may help lower lipoprotein (a)
L-carnitine can lower lipoprotein(a) (Lp(a)) levels by about 20%. A meta-analysis of randomized controlled trials found that oral L-carnitine supplementation significantly lowered plasma Lp(a) levels by a weighted mean difference (WMD) of -8.82 mg/dL
If you decide to try L-carnitine it is important to have your TMAO blood levels checked.
Coenzyme Q10
Randomized trial
A randomized, double-blind, placebo-controlled trial found that CoQ10 supplementation significantly reduced Lp(a) levels in patients with acute coronary disease.
Systematic review
A systematic review and meta-analysis found that CoQ10 supplementation consistently reduced Lp(a) levels across different dose
Indian gooseberry (amla) may help lower lipoprotein a (Lp(a)) levels. A pilot study found that amla extract significantly reduced Lp(a) levels, along with other cholesterol markers. However, some say that the evidence supporting this claim is questionable because studies funded by amla supplement companies may have conflicts of interest.
How to Lower Lp(a) with Diet
https://www.youtube.com/watch?v=Up0YORTEr50
Dr. Grisanti's Comments:
Everything you need to know about Lp(a) by Dr. Thomas Dayspring
https://www.youtube.com/watch?v=-WRRyG8il4g
Thomas Dayspring Bio
“We can't treat what we don't measure, and we hope these findings move the field closer to identifying even earlier ways to detect and prevent heart disease,” said Paul M. Ridker, M.D., M.P.H., a study author and the director of the Center for Cardiovascular Disease Prevention at Brigham and Women's Hospital, Boston.
My final comment is to get aggressive in lowering these three cardiovascular markers: LDL cholesterol, high sensitivity C-Reactive Protein and Lipoprotein (a).
I recommend reviewing my past articles on cardiovascular disease:
Understanding The Three-Legged Stool Concept to Winning the War on Cardiovascular Disease
https://www.functionalmedicineuniversity.com/public/1998.cfm
Lipopolysaccharide (LPS) and the Incidence of Cardiovascular Disease
https://www.functionalmedicineuniversity.com/public/1985.cfm
Why Apolipoprotein B (ApoB) May Be a Better Predictor of Your Heart Disease Risk
https://www.functionalmedicineuniversity.com/public/1984.cfm
Trimethylamine N-oxide (TMAO)-- An Underrated Yet Important Cardiovascular Lab Marker
https://www.functionalmedicineuniversity.com/public/1963.cfm
ATTENTION DOCTORS, ALL HEALTHCARE PRACTITIONERS, PATIENTS and POTENTIAL NEW PATIENTS
If you found this article of value may I ask if you can tell your friends and colleagues about Clinical Rounds. This is a great introduction to the field of functional medicine as well as having the opportunity to stay current on the latest medical news on a variety of important health issues.
Here is the webpage to subscribe:
http://www.clinicalrounds.com
WOULD YOU BE INTERESTED IN EARNING YOUR CERTIFICATION IN FUNCTIONAL MEDICINE?
Functional Medicine University (FMU) has been training and certifying healthcare professionals since 2006. With over 8000 students in all 50 states and 68 countries you have a unique opportunity to help hundreds to thousands of patients suffering with a variety of health challanges.
To Learn More About FMU go to: https://www.functionalmedicineuniversity.com/
We Accept 150 New Students Every 90 Days.
If you are ready to obtain your certification in functional medicine I would encourage you to reserve your seat by going to:
https://www.functionalmedicineuniversity.com/public/enrollment.cfm
References:
https://www.nhlbi.nih.gov/news/2024/lipoproteina-what-know-about-elevated-levels
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1336715/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2891301/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2891301/
https://pubmed.ncbi.nlm.nih.gov/16646631/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3671388/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5872797/
https://www.sciencedirect.com/science/article/pii/S0022316623006946
https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2819335
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5561768/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7363506/
9/10/24, 8:57 AM 3 Blood Tests Can Warn Women of Risk 30 Years before Heart Attack and Stroke | Functional Medicine University - The Leader in Online Training in Functional Diagnostic Medicine
https://www.functionalmedicineuniversity.com/public/2053print.cfm 4/5
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5345575/
https://pubmed.ncbi.nlm.nih.gov/31519281/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1456807/
https://www.sciencedirect.com/science/article/pii/S0022316622096778
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4924162/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8308638/
https://www.sciencedirect.com/science/article/abs/pii/S0149291821003969
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6040119/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2631578/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2631578/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9751896/
https://academic.oup.com/milmed/article/179/suppl_11/2/4210235
https://www.ahajournals.org/doi/10.1161/ATV.0000000000000147
https://www.ahajournals.org/doi/10.1161/CIRCULATIONAHA.118.037184
https://pubmed.ncbi.nlm.nih.gov/20842562/
https://pubmed.ncbi.nlm.nih.gov/30055165/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4709689/
https://pubmed.ncbi.nlm.nih.gov/11213533/
https://www.jacc.org/doi/10.1016/S0735-1097%2816%2932033-2
https://www.mdpi.com/2077-0383/13/3/751
https://pubmed.ncbi.nlm.nih.gov/26836888/
https://www.sciencedirect.com/science/article/abs/pii/S1043661815302231
https://pubmed.ncbi.nlm.nih.gov/10077397/
https://www.mdpi.com/2077-0383/13/3/751
https://pubmed.ncbi.nlm.nih.gov/15172426/
https://www.webmd.com/heart-disease/features/can-you-reverse-coronary-artery-disease
https://www.sciencedirect.com/science/article/pii/S0735109704007168
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6491397/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10222947/
https://pubmed.ncbi.nlm.nih.gov/28364865/
** Always consult with a physician or healthcare practitioner with significant integrative or functional medicine training before starting any of the above recommendations.
You can find a qualified and certified functional medicine practitioner by going to: www.FunctionalMedicineDoctors.com
The information on this website is not intended to replace a one-on-one relationship with a qualified health care professional and is not intended as medical advice. It is intended as a sharing of knowledge and information from the research and experience of Dr. Grisanti and his functional medicine community. Dr. Grisanti encourages you to make your own health care decisions based upon your research and in partnership with a qualified health care professional. Visit www.FunctionalMedicineUniversity.com for more information on our training in functional medicine. Look for practitioners who have successfully completed the Functional Medicine University's Certification Program (CFMP) www.functionalmedicinedoctors.com. This content may be copied in full, with copyright, contact, creation and information intact, without specific permission, when used only in a not-for-profit format. If any other use is desired, permission in writing from Dr. Grisanti is required
Send a Message
Experience the power of holistic healing. Let us help you discover the root cause of your chronic pain and embark on a journey towards lasting relief and optimal well-being. Contact us now to start your transformation!
Get in Touch
Phone number
(720) 902-9200